Kidney Failure Treatment Without Dialysis
Alternative Approaches to Kidney Failure Management
Kidney Failure Treatment Without Dialysis – Introduction
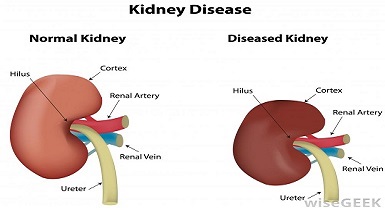
What is Renal Failure?
Renal failure or kidney failure occurs when your kidneys don’t work properly. Think of your kidneys as filters that clean your blood by removing waste and extra fluids to keep you healthy. When they don’t work well it can lead to issues like swelling, fatigue, and a buildup of waste in your body, known as toxins.
Renal failure, also known as end-stage renal disease (ESRD) is a serious condition that requires renal replacement therapy to sustain life. While dialysis is a commonly used treatment modality for kidney failure, it may not be suitable for all patients due to various reasons such as medical complications, patient preference, or limited access to dialysis facilities.
In this comprehensive analysis, we will explore non-dialysis treatment options for kidney failure and delve into recent research studies that highlight alternative approaches in managing this challenging condition. Join us on this journey as we uncover the potential benefits and limitations of non-dialysis treatment strategies.
Conservative Management in Kidney Failure
Conservative management, also known as supportive care or medical management, is an approach that focuses on optimizing the patient’s quality of life while managing symptoms and complications associated with kidney failure. Research studies, including those conducted by Roderick et al. (2009) and Chandna et al. (2018), have explored the outcomes and challenges of conservative management in kidney failure patients.
Conservative management involves close monitoring of the patient’s condition, dietary modifications, medication management, and control of underlying medical conditions such as hypertension and diabetes. The goal is to slow down the progression of kidney disease, manage symptoms such as fluid retention and electrolyte imbalances, and provide comfort and support to the patient.
While conservative management does not replace the function of the kidneys, it can be a viable option for select patients, particularly those with advanced age, significant comorbidities, or a limited life expectancy. Research has shown that conservative management can provide comparable or even better outcomes in terms of quality of life, survival rates, and cost-effectiveness compared to dialysis in specific patient populations.
Kidney Transplantation as a Non-Dialysis Treatment Option
Kidney transplantation is considered the gold standard treatment for end-stage renal disease, offering the potential for long-term kidney function restoration and improved quality of life. Extensive research studies, including those by Wolfe et al. (2016) and Hart et al. (2019), have examined the outcomes and advancements in kidney transplantation for kidney failure patients.
Transplantation involves the surgical placement of a healthy kidney from a living or deceased donor into a recipient with kidney failure. The transplanted kidney assumes the function of the failed kidneys, allowing the patient to regain kidney function and eliminate the need for dialysis. It offers several advantages, including better survival rates, improved quality of life, and freedom from the restrictions and complications associated with dialysis.
Advancements in transplantation techniques, immunosuppressive medications, and organ preservation have significantly improved transplant outcomes over the years. Research continues to focus on optimizing donor-recipient matching, reducing rejection rates, and improving long-term graft survival.
However, it is important to note that kidney transplantation is not suitable for all patients due to factors such as availability of suitable donors, medical eligibility, and patient preference. The limited supply of donor organs and the need for lifelong immunosuppression are significant challenges associated with transplantation. Thus, alternative non-dialysis treatment options are essential for patients who are not transplant candidates or face barriers to transplantation.
Peritoneal Dialysis as an Alternative Non-Dialysis Treatment Option
Peritoneal dialysis (PD) is a form of renal replacement therapy that can be performed at home, offering flexibility and independence to patients with kidney failure. Research studies, including those conducted by Brown et al. (2019) and Mehrotra et al. (2020), have investigated the effectiveness and advantages of peritoneal dialysis as an alternative to conventional hemodialysis.
PD involves the use of the peritoneal membrane in the abdomen as a natural filter. A dialysis solution is introduced into the peritoneal cavity, and waste products and excess fluids are removed through osmosis and diffusion. PD can be performed using automated peritoneal dialysis (APD) machines or manual exchanges, depending on the patient’s needs and capabilities.
PD offers several advantages over hemodialysis, including a more gradual and continuous removal of toxins, better preservation of residual kidney function, fewer dietary restrictions, and the ability to perform dialysis at home. Research has shown that PD can provide comparable outcomes in terms of patient survival, quality of life, and cost-effectiveness compared to hemodialysis.
However, PD may not be suitable for all patients, as it requires a suitable peritoneal membrane, adequate manual dexterity, and a safe and clean environment for performing exchanges. Careful patient selection, education, and ongoing monitoring are essential for successful PD implementation.
Emerging Therapies and Future Directions
Advancements in research and technology continue to pave the way for innovative non-dialysis treatment options for kidney failure. Several promising therapies and approaches are currently under investigation, aiming to improve kidney function, slow disease progression, or enhance the effectiveness of existing treatment modalities.
One such area of research is regenerative medicine and tissue engineering, which explores the potential of growing functional kidney tissue in the laboratory for transplantation or implantation. Researchers are investigating methods to stimulate the regeneration of damaged kidney tissue using stem cells, growth factors, and biomaterials.
Another area of focus is the development of novel pharmacological interventions that target specific mechanisms involved in kidney damage and disease progression. Research studies are exploring the use of agents that can modulate inflammation, oxidative stress, fibrosis, and immune responses to preserve renal function and delay the need for dialysis.
Furthermore, wearable and implantable devices, such as wearable artificial kidneys and bioartificial renal tubules, are being developed to provide continuous renal support and mimic the functions of the native kidneys. These technologies aim to improve patient mobility, enhance dialysis efficiency, and reduce the burden of conventional dialysis treatments.
Conclusion
Non-dialysis treatment options for kidney failure, such as conservative management, kidney transplantation, and peritoneal dialysis, offer viable alternatives to conventional dialysis. Each approach has its advantages, considerations, and limitations, and the choice of treatment should be individualized based on the patient’s medical condition, preferences, and available resources.
Ongoing research continues to expand our understanding of kidney failure and open new avenues for innovative non-dialysis treatment options. By staying at the forefront of scientific advancements and leveraging interdisciplinary collaborations, we can strive towards improving patient outcomes, enhancing quality of life, and reducing the burden associated with end-stage renal disease.