Causes of Chronic Renal Failure
Chronic Renal Failure Introduction
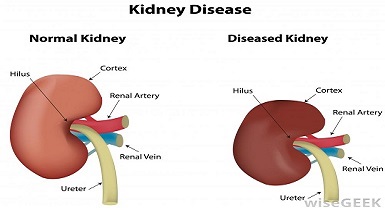
Chronic renal failure, also known as chronic kidney disease (CKD), is a progressive condition characterized by the gradual loss of kidney function over time. It affects millions of people worldwide and is associated with significant morbidity and mortality. In this interactive blog, we will delve into the causes of chronic renal failure and explore recent research studies that provide valuable insights into this complex condition. Join us on this journey as we unravel the contributing factors and advancements in the field.
Diabetes Mellitus and Chronic Renal Failure
Diabetes mellitus, both type 1 and type 2, is a leading cause of chronic renal failure. The high blood sugar levels associated with diabetes can damage the small blood vessels in the kidneys, leading to renal dysfunction. Research studies, such as those conducted by Tonneijck et al. (2017) and Thomas et al. (2020), have shed light on the pathophysiological mechanisms linking diabetes and chronic renal failure.
To gain a deeper understanding, let’s explore the impact of glycemic control on kidney health. Poorly controlled blood sugar levels contribute to the development and progression of renal damage. High glucose levels result in the production of reactive oxygen species (ROS) and the activation of inflammatory pathways, leading to oxidative stress and chronic inflammation in the kidneys. These processes ultimately contribute to renal dysfunction.
Additionally, the renin-angiotensin-aldosterone system (RAAS), a key regulator of blood pressure, plays a significant role in diabetic kidney disease. Research has shown that medications targeting the RAAS, such as angiotensin-converting enzyme inhibitors (ACE inhibitors) and angiotensin receptor blockers (ARBs), can slow the progression of renal damage in individuals with diabetes.
Hypertension and Chronic Renal Failure
Hypertension, or high blood pressure, is a significant risk factor for chronic renal failure. The sustained elevation in blood pressure can damage the blood vessels in the kidneys, impairing their ability to effectively filter waste products. Several research studies, including those by Brenner et al. (2001) and Taler et al. (2021), have investigated the intricate relationship between hypertension and chronic renal failure.
To better understand the connection, let’s delve into pathophysiology. Persistent high blood pressure causes structural changes in the renal vasculature, leading to a decrease in renal blood flow and subsequent tissue damage. The kidneys’ ability to filter waste products and regulate fluid and electrolyte balance becomes compromised, contributing to the development of chronic renal failure.
Management of hypertension plays a crucial role in preventing or delaying the progression of chronic renal failure. Medications that inhibit the RAAS, such as ACE inhibitors and ARBs, are commonly prescribed to individuals with hypertension and CKD. These medications help lower blood pressure and reduce the pressure exerted on the kidneys, thus protecting renal function.
Glomerular Diseases and Chronic Renal Failure
Glomerular diseases, such as glomerulonephritis and focal segmental glomerulosclerosis (FSGS), can lead to chronic renal failure. Recent research, including studies by Waldman et al. (2015) and Appel et al. (2019), has identified genetic and immune-mediated factors contributing to glomerular diseases and subsequent renal dysfunction.
To grasp the underlying mechanisms, let’s explore the role of the immune system in glomerular diseases. In certain individuals, abnormal immune responses lead to inflammation and damage to the glomeruli, the tiny filtering units in the kidneys. This can be due to genetic factors
or an autoimmune response where the body’s immune system mistakenly attacks the kidney tissue.
Research has shown that specific immune-related proteins, such as complement proteins, play a crucial role in glomerular diseases. Dysregulation of the complement system can trigger inflammation and injury to the glomeruli. Understanding these immune-mediated processes is vital for developing targeted therapies to manage glomerular diseases and preserve renal function.
Infections and Chronic Renal Failure
Infections, both systemic and urinary tract infections (UTIs), can contribute to chronic renal failure. Chronic pyelonephritis, a recurrent kidney infection, can cause progressive damage to the renal tissue. Additionally, certain viral infections, such as hepatitis B and hepatitis C, have been associated with an increased risk of chronic renal failure. Research studies, such as those conducted by Goicoechea et al. (2015) and Fabrizi et al. (2020), have examined the relationship between infections and chronic renal failure.
Let’s explore the impact of urinary tract infections on kidney health. UTIs can lead to kidney infection if left untreated or if bacteria ascend from the bladder to the kidneys. The infection causes inflammation and scarring in the renal tissue, impairing its function. Recurrent UTIs can further exacerbate kidney damage over time.
Certain viral infections, such as hepatitis B and hepatitis C, have been associated with glomerular diseases and chronic renal failure. The viruses can directly infect the kidney cells or trigger an autoimmune response, leading to kidney damage. Identifying and treating these viral infections promptly is crucial for preserving renal function.
Medications and Environmental Toxins in Chronic Renal Failure
Certain medications and environmental toxins can contribute to kidney damage and chronic renal failure. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), certain antibiotics, and certain chemotherapeutic agents can have nephrotoxic effects. Research studies, including those by Perazella (2019) and Mutsaers et al. (2020), have shed light on the mechanisms of drug-induced nephrotoxicity.
Environmental toxins, such as heavy metals (e.g., lead, mercury, and cadmium), pesticides, and certain solvents, can also pose a risk to kidney health. Prolonged exposure to these toxins can lead to renal dysfunction. Research studies have examined the impact of environmental toxins on kidney health, highlighting the importance of environmental awareness and regulation to prevent kidney damage.
Genetic and Congenital Factors in Chronic Renal Failure
Genetic factors play a significant role in the development of chronic renal failure. Inherited conditions such as polycystic kidney disease (PKD) and Alport syndrome can lead to progressive renal dysfunction. Research studies, including those conducted by Cornec-Le Gall et al. (2020) and Bekheirnia et al. (2021), have identified specific gene mutations associated with these conditions.
Polycystic kidney disease, the most common inherited kidney disorder, is characterized by the formation of fluid-filled cysts in the kidneys. These cysts gradually enlarge and impair kidney function over time. Alport syndrome, on the other hand, is a genetic disorder that affects the glomeruli and can lead to renal failure.
Understanding the genetic basis of chronic renal failure is crucial for developing targeted therapies and personalized treatment approaches. Research efforts are focused on identifying genetic markers and understanding the underlying mechanisms to improve the management of genetic and congenital causes of chronic renal failure.
Conclusion
Chronic renal failure has various causes, including diabetes mellitus, hypertension, glomerular diseases, infections, medications, and genetic factors. Understanding the underlying
mechanisms and risk factors associated with chronic renal failure is crucial for developing effective preventive strategies and treatment modalities. Ongoing research continues to shed light on this complex field, with advancements in genetics, immunology, pharmacology, and environmental awareness offering promising avenues for mitigating kidney damage and improving patient outcomes.
As we uncover the intricacies of chronic renal failure, it becomes evident that a multidisciplinary approach, involving nephrologists, endocrinologists, geneticists, and other healthcare professionals, is essential for comprehensive management. By staying informed about the latest research findings, we can work towards improving early detection, implementing preventive measures, and developing innovative therapies to alleviate the burden of chronic renal failure worldwide.